
Injuries are an unfortunate part of sport. How an athlete recovers from an injury can determine their future success. Often the rehabilitation and return to sport programs are progressed in silos between the MD, PT, ATC, and S&C. To no fault of their own each domain has their own historical check points they follow for certain injuries. However, it is our perspective that rehabilitating an athlete from injury should be a more collaborative, data driven process. Training direction, progression decisions, and clearance should be based on key objective markers and the athlete’s unique biomechanical profile.

Too much of the attention surrounding injuries in sport occurs after the injury has happened. At P3 we believe that frequent screenings can not only serve as effective benchmarks in the unfortunate scenario in which an athlete does get injured, but preemptive screenings also give us the opportunity to identify risky mechanics and apply interventions before an injury occurs.
In elite sport most teams have healthy baseline “training loads” from practice or games. This data can be used to gradually build athletes to their preinjury workloads and gauge their distance from personal averages across a variety of accelerative metrics. Though valuable this type of data does not provide much insight into “how” these loads are being accumulated. In fact, athletes are historically known for being good compensators and the simple fact that they can reach game speed again does not mean that they are game ready.
Healthy baseline biomechanical data can provide teams with criterion loading and propulsive asymmetries across a variety of plyometric movements. These kinetic and kinematic values can orient training goals and supplement on court, on field outputs to gauge an athlete’s true progress. Furthermore, pairing kinetic outputs with kinematic data from the lower extremities during plyometric movements allows us to take a more granular look at how an athlete may be compensating post injury, and how these compensations are trending over time. Though baseline jump outputs may be achieved in some cases injurious mechanics present themselves as well.
In the event where a team does not have healthy baseline data, but an athlete still gets injured, 3D biomechanical assessments can still play a vital role in return to play. Regressed movements can be performed at greater frequency to measure factors such as time to stabilization upon landing, loading kinetics, propulsive kinetics, and joint rotations. These data points can inform the rehab and S&C staff of an athlete’s progress and allow for targeted real time interventions.
In any form contextualized 3D biomechanical data can bring everyone (MD’s, PT’s, ATC’s, and S&C’s) to the same table speaking the same language, keeping the athlete’s best interest in mind. Key metrics can serve as benchmarks to guide rehab and return to play protocols in a more objective matter.
CASE STUDY
NBA PLAYER: ACL RETURN TO PLAY
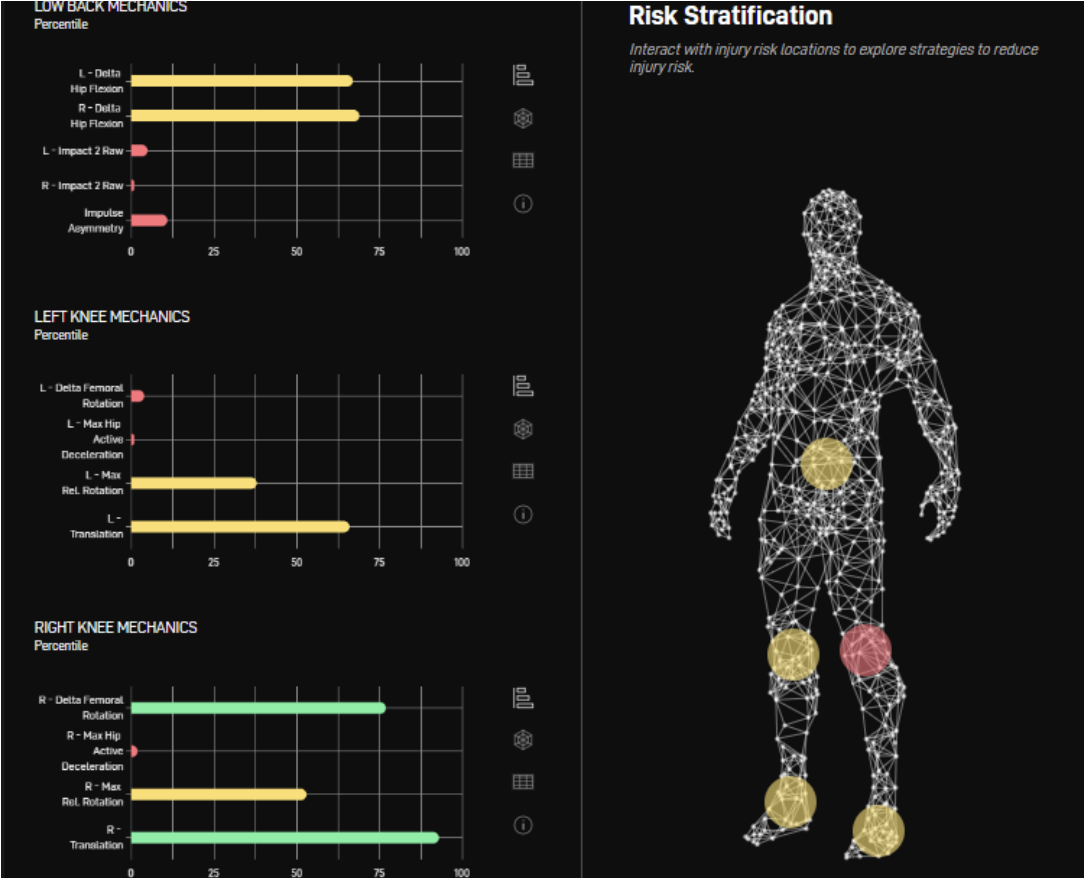
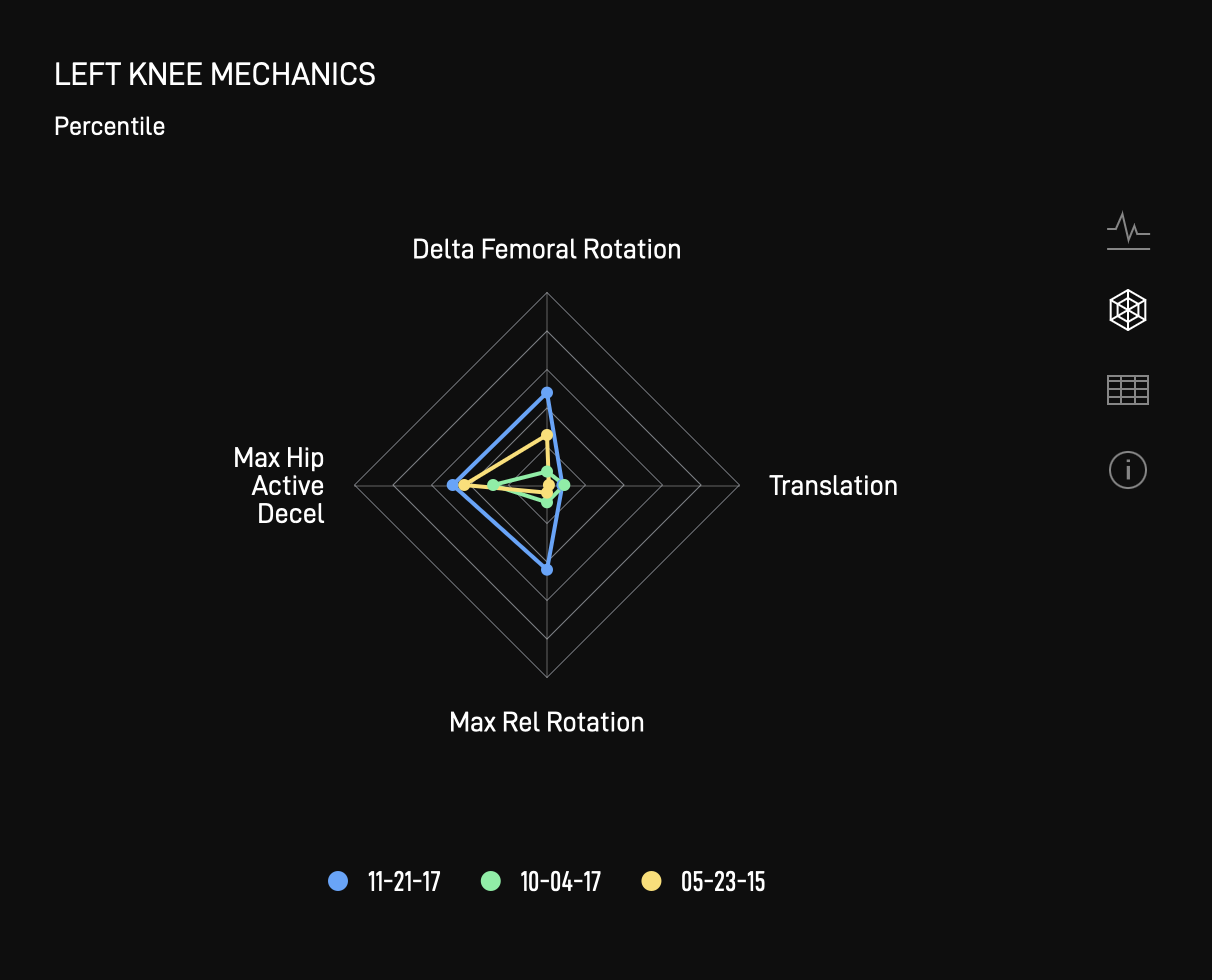
During athlete’s initial assessment, P3’s injury risk indicators flag the athlete as being at elevated risk of traumatic knee injury to the left side as a result of excessive Delta Femoral Rotation and a Lack of Hip Deceleration. The Athlete, shortly after the assessment suffered a non-contact ACL rupture to the left side.
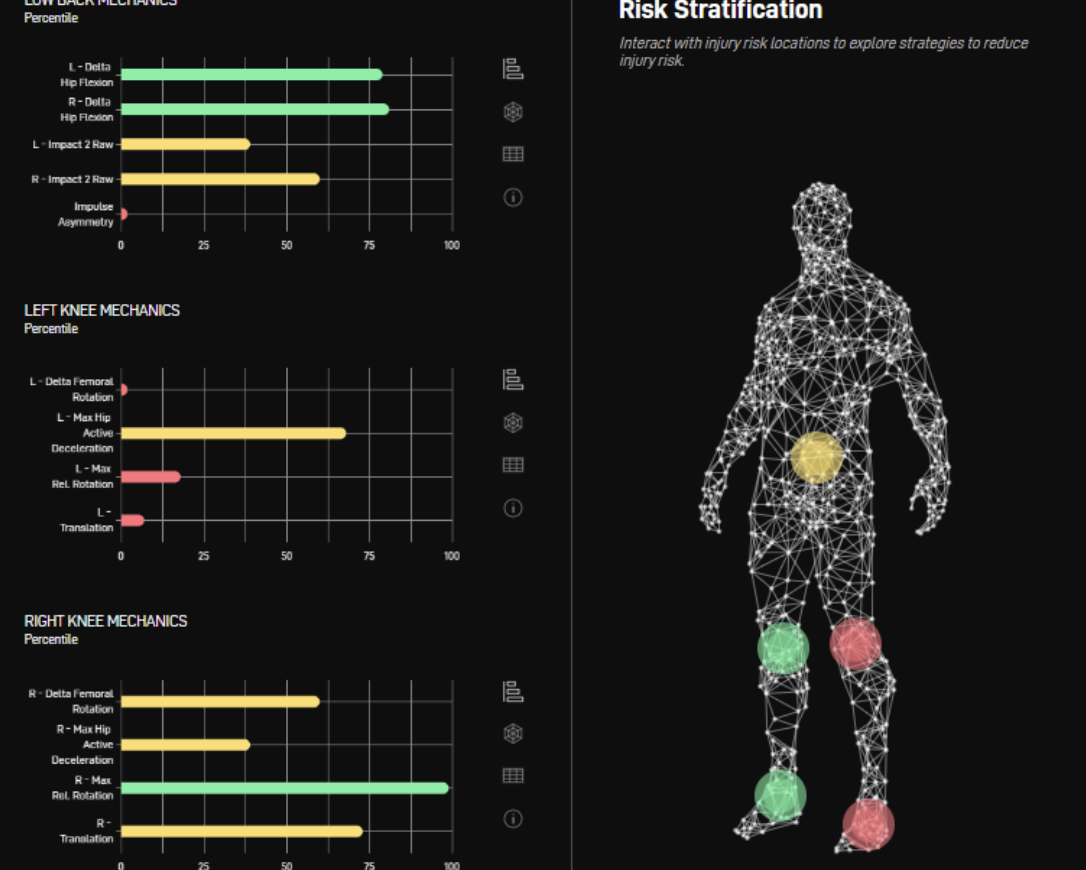
9 months post operation, the athlete is jumping just as high as before injury, but continues to exhibit “risky” mechanics. P3 helps the athlete’s team develop a tailored training intervention to address underpinning risk factors.
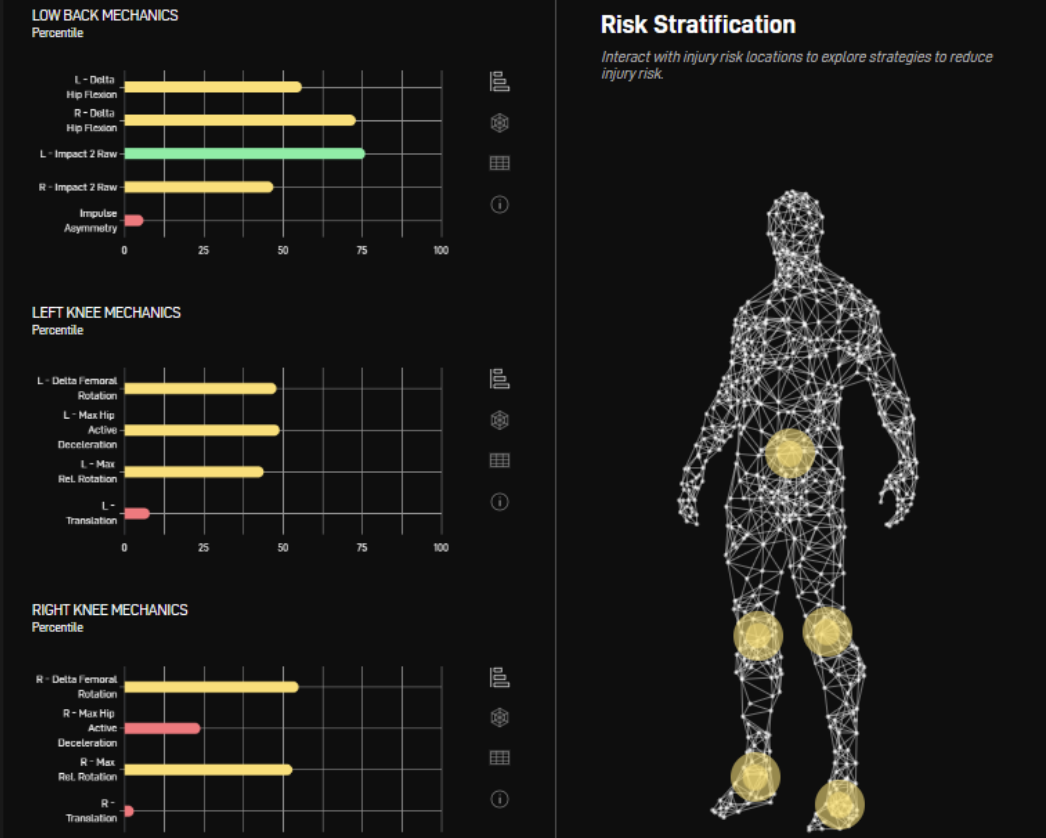
11 months post operation, following a tailored training intervention and progressive exposure to basketball activities, the athlete is now exhibiting mechanics that place him in a more normal risk zone without sacrificing performance. The athlete has since become an all star and has not suffered any further significant lower extremity injuries.